
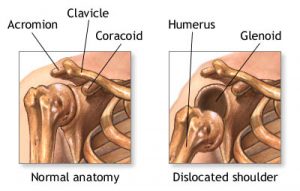
Shoulder dislocations are more appropriately referred to as glenohumeral dislocations. Glenohumeral dislocations are part of a broad spectrum of shoulder disorders related to instability of this joint. There is no true shoulder joint, but the ball and socket joint called the glenohumeral joint is thought of as the true shoulder joint by most people. The glenoid or socket is very shallow. The anatomic relationship is like a golf ball sitting on a tee. The ball represented by the head of the humerus, and the tee represented by the glenoid of the shoulder blade. The problem is that the tee is placed on its side and angled forward. The glenoid surface is surrounded by a lip of fibrocartilage known as the labrum. This deepens the socket for the humerus and augments stability of this joint. There is significant individual variation in the amount of ligamant laxity and consequent movement at this joint. People with generalized ligament laxity, especially young women, tend to have a great deal of potential movement of the ball in the socket. The ball can move freely in most directions, especially forward and inferiorly. Because of muscle imbalance, the ball frequently sits towards the front of the socket, and this is often associated with irritation of the biceps tendon and the infraspinatus muscle of the rotator cuff, located on the back of the shoulder blade.
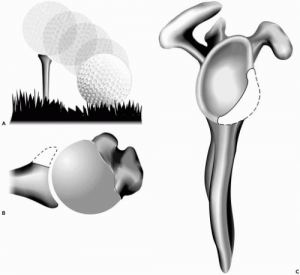
The glenoid is very shallow, like a golf tee in relationship to the much larger ball….
Shoulder instability can be categorized as either “T.U.B.S.” or “A.M.B.R.I.”
Historically, we have lumped two main patient groups together based on those that have stable shoulders and those that have unstable shoulders. Those that have stable shoulders who dislocate their shoulder are described as having a “T.U.B.S.” type of pathology. This stands for Traumatic, Unilateral, Bankart lesion and Surgery. To breakdown this acronym, individuals who dislocate their shoulder typically have a violent mechanism of injury if they have a normally stable shoulder. The mechanism of injury is typically one of external rotation and abduction of the arm, where it goes up towards the side. This position would be frequently encountered in a thrower.
The “U” stands for “Unilateral”, in that most patients only experience this on one side of their body. Most dislocations go in an anterior direction. So the “U” can also mean unidirectional. The “B” refers to a “Bankart lesion” which is a term applied to a tear of the labrum or fibrocartilage, typically at the bottom of the socket. The labrum is torn as the ball violently exits the socket. The “S” part of the acronym accounts for “Surgery” in that there is high level evidence that individuals who have glenohumeral dislocations have a better prognosis if they have stabilization surgery early in their course. Not all jurisdictions practice this way, however.
Another large group of shoulder dislocators are those who are described as having “A.M.B.R.I.” types of instability. The “A” refers to “Atraumatic” in that the shoulder can pop out of joint with very little force. The “M” stands for “Multidirectional” where the patients often have excessive motion forward, inferiorly, as well as backward. This is called multidirectional glenohumeral laxity. The “B” stands for “Bilaterality” indicating that this is something that happens to both shoulder joints. The “R” stands for “Rehabilitation” as these people do not fare as well with shoulder surgery. The “I” stands for “Intensive rehabilitation” which is often required in these individuals, and “Inferior capsular shift”, one of the historical operations in this group of patients.
A patient with an acute shoulder dislocation is usually in a great deal of distress and attends an Urgent Care or Emergency Centre.
In general, when an individual dislocates their shoulder, they require expert medical help relocating it. An x-ray needs to be done to confirm the pathology. Traction on the arm with some external rotation to the hand is typically required to relocate the joint. Counter traction has to be applied through the armpit. The use of medications that can relax an individual such as Midazolam greatly facilitate the reduction process, and this has to be administered in the Emergency Room.
After the joint is x-rayed back in place, the individual can proceed with some short term immobilization for comfort. Although there is no absolute timeframe for immobilization, younger patients tend to be immobilized somewhat longer hoping to augment the stability of the joint, whereas older patients often need to be mobilized early to prevent excessive stiffness of the shoulder joint. Unfortunately, in this population, “old” is over the age of 40. Those over 40 frequently can be mobilized quickly.
As part of the rehabilitation process, the individual needs to go through both mobilization exercises to gain range of motion and strengthening exercises to help augment the ball-socket stability. Please see the shoulder rehabilitation video section for stability exercises for the ball socket joint. If a person has a recurrence and they tend to have the “TUBS” type of pathology, then early surgical consultation is warranted. Surgery in patients with multi-directional laxity needs to be given sober consideration, as outcomes are less favourable.
Exercises for shoulder mobility and stability are required in the rehabilitation process…the bosu ball push up is a great stability exercise

